- Counseling
- Nursing
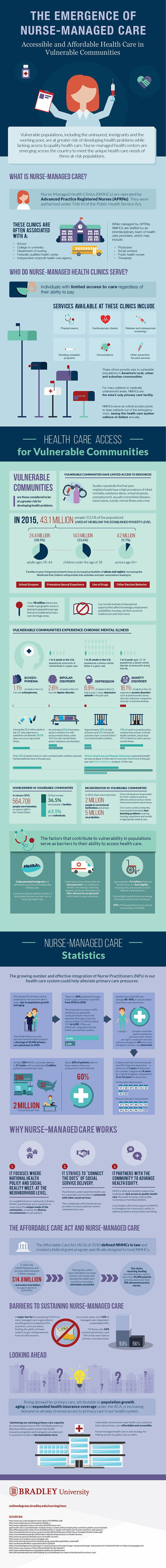
The Emergence of Nurse-Managed Care: Providing Accessible, Affordable Health Care in Vulnerable Communities
Vulnerable populations, including the uninsured, immigrants and the working poor, are at greater risk of developing health problems while lacking access to quality health care. Nurse-managed health centers are emerging across the country to meet the unique health care needs of these at-risk populations. To learn more, check out the infographic below created by Bradley University's online Master's in Nursing program.
Add This Infographic to Your Site
<p style="clear:both;margin-bottom:20px;"><a href="https://onlinedegrees.bradley.edu/blog/nurse-managed-health-centers" rel="noreferrer" target="_blank"><img src="https://res.cloudinary.com/dqtmwki9i/image/fetch/https://www.project-alpine.com/assets/d75a33dd-2f54-4ac7-adf5-23546b3b3d2c" alt="Infographics on the Emergence of Nursed-Managed Care and Providing Accessible Affordable Health Care in Vulnerable Communities" style="max-width:100%;" /></a></p>An Overview of Nurse-Managed Care
Authorized by Title III of the Public Health Service Act and managed by Advanced Practice Registered Nurses (APRNs), nurse-managed health clinics (NMHCs) serve people who are unable to access or afford good health care services. NMHCs generally are associated with institutions such as colleges/universities, federally approved medical centers and health agencies. Some of the health professionals who work in these facilities include therapists, doctors, nurses and social workers.
Population Demographic Served by NMHCS
NMHCs normally are established to serve people who cannot access health care services at conventional medical facilities both in urban and rural settings across the U.S. The facilities offer a wide range of health care services, including immunizations, physical exams, diabetes and osteoporosis screenings, addiction programs and cardiovascular checks. It is important to note that the medical services offered at these facilities typically are focused on disease prevention rather than treatment. As such, these facilities help to prevent serious health complications and save the health sector billions of dollars annually.
How the Vulnerable Communities are Disadvantaged in Terms of Health Care
Vulnerable populations in the U.S. mostly are found in low-income neighborhoods that are plagued by high high school dropout rates, high levels of crime and substance abuse, and high suicide, infant mortality and unemployment rates. This environment makes these groups prone to health complications. Even worse, these groups cannot afford the health care services they need. By the end of 2015, the U.S. was home to approximately 43.1 million people living below the national poverty level. Of these individuals, 24.4 million were adults ages 18 to 64 and 14.5 million were teens and children 18 years and younger, while 4.2 million were seniors age 65 years and over.
Although adults can survive in such communities, children are the most disadvantaged, with most likely to experience neglect as well as physical and sexual abuse. Additionally, schoolchildren often are prone to peer pressure, thereby increasing their likelihood of dropping out. Both boys and girls also are prone to premature sexual experiences, which in turn increases the risk of teenage pregnancies in girls. In urban centers, gangs thrive and expose their communities to gun violence. Finally, members of vulnerable groups are generally more prone to deviant behavior, including illegal drug use.
Currently, more than 58 million Americans live in areas/communities where they cannot easily access medical care. Lack of employment, minimal housing opportunities and high illiteracy rates make it even harder for people in vulnerable communities to access health services.
Mental Health among the Vulnerable Groups
Vulnerable populations are more likely to develop mental health issues compared to any other demographic. At present, one in every five American adults experiences mental health problems annually, while one in every 25 adults experiences serious health issues at some point over the same period. This number is in addition to one in every five youths who experience serious mental health difficulties at some point in life. Anxiety disorders such as posttraumatic stress disorder and obsessive-compulsive disorder affect 18.1 percent of the adult population while 6.9 percent of American adults suffer from depression. At least 2.6 percent of adults have bipolar disorder, and 1.1 percent of adults live with schizophrenia.
For adults with drug dependency issues, 50.5 percent experience co-occurring mental health problems. Moreover, 26 percent of homeless adults already have serious mental illnesses while 46 percent of the same demographic are struggling with substance abuse disorders. The justice system faces similar problems with 20 percent of state prisoners and 21 percent of local jail prisoners having experienced mental health problems in the recent past. Youths in juvenile justice facilities are the worst affected with 70 percent having experienced at least one mental health challenge. At the same time, 20 percent of juvenile offenders have serious mental illnesses. Only 41 percent of American adults with mental illnesses have received proper care in the last one year. In particular, African-Americans and Hispanic-Americans only received medical care at half the rate of Caucasians and one-third the rate of Asian-Americans.
Homelessness and Incarceration
The U.S. had 564,708 homeless people in January 2015. Of these people, 63.5 percent were individuals while 36.5 percent were families. Vulnerable communities also are prone to incarceration, with 2 million individuals locked up in correctional facilities and 5 million on probation.
Nurse-Managed Care by the Numbers
The U.S. health care system will face a shortage of 20,400 primary care givers by 2020. On the other hand, the number is nurse practitioners (NPs) is expected to rise by 30 percent to cut staff shortage in the NMHC niche to just 6,400 over the same period. Luckily, research has shown that NPs can provide 80–90 percent of the health care currently provided by traditional physicians. To date, about 200 NMHCs have been opened across the U.S., providing medical care to roughly 2 million patients every year. Up to 60 percent of patients who visit NMHCs are uninsured. Unlike doctors, NPs complete their training within seven to eight years.
The Benefits of NMHCs
NMHCs provide much-needed health services at the community level (where other medical professionals cannot reach). Furthermore, NMHCs enable health professionals to collaborate with social services to improve service delivery. NMHCs also enable health professionals to build rapport within communities where they work.
NMHCs and Affordable Care Act
The Affordable Care Act (ACA) covers NMHCs and provides funding to run some programs. For instance, ten NMHCs that provide medical care to over 94,000 patients received $14.8 million from the Health Resources & Services Administration in 2010. These funds were used to improve access to primary care services and the outcome has been a resounding success.
Challenges Faced by NMHCs
Managed-care providers have been unwilling to offer NPs the relevant credentials, making it hard to receive reimbursements from private insurance companies. Only 53 percent of managed-care providers have employed credentialed NPs.
The Future of NMHCs
Demand for primary health care will continue to rise in the near future due to a growing elderly population and universal health coverage. This fact means more effort must be made to boost the capacity of primary care givers.
Recommended Reading
Nurse Practitioners: Improving Quality of Care and Saving Costs
Career Spotlight: Pediatric Nurse Practitioner
Bradley University Online MSN-FNP Program
