- Counseling
- Nursing
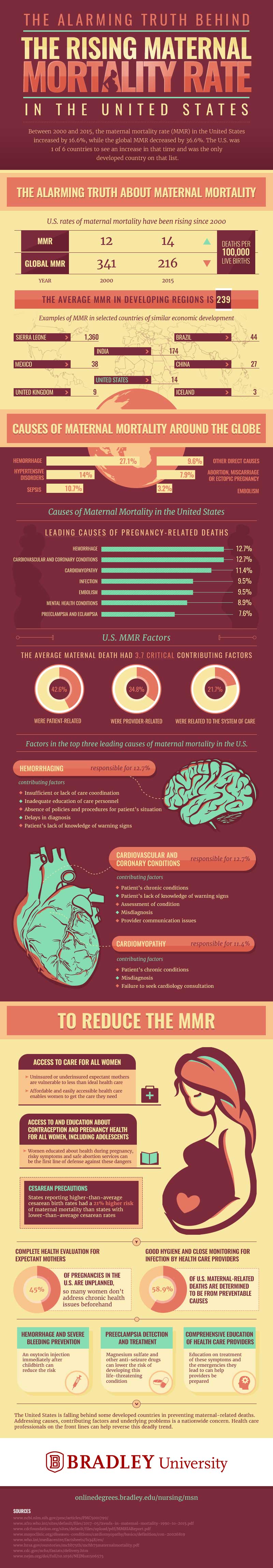
The Alarming Truth Behind the Rising Mortality Rate in the U.S.
While the global maternal mortality rate (MMR) decreased by 36.6 percent between 2000 and 2015, the U.S. MMR increased by 16.6 percent. The United States was one of six countries and the only developed country to see an increase in maternal mortality during this time period.
To learn more, check out the infographic below designed by Bradley University’s online Master of Science in Nursing program.
Add This Infographic to Your Site
<p style="clear:both;margin-bottom:20px;"><a href="https://onlinedegrees.bradley.edu/blog/maternal-mortality-rate" rel="noreferrer" target="_blank"><img src="https://res.cloudinary.com/dqtmwki9i/image/fetch/https://www.project-alpine.com/assets/ae4b9ae9-2c65-43a7-b4a3-3d97eb227678" alt="The alarming truth behind the rising maternal mortality rate in us final" style="max-width:100%;" /></a></p>The Alarming Truth about Maternal Mortality
The U.S. maternal mortality rate has been rising since 2000. There were 12 deaths for every 100,000 live births in 2000, and this rate has risen to 14 out of 100,000 live births by 2015.
In contrast, the global maternal mortality rate has been decreasing steadily since 2000. While there were 341 deaths for every 100,000 live births around the world in 2000, there were only 216 deaths for every 100,000 live births worldwide by 2015.
In developing regions, the average rate of maternal mortality is 239. Sierra Leone has an especially high MMR, with 1,360 deaths per 100,000 live births. India also has a fairly high maternal mortality rate, with 174 deaths reported for every 100,000 live births.
In developed regions, the average rate of maternal mortality is comparatively low. The United Kingdom has an average of 9 deaths per 100,000 live births, and Iceland has an average of only 3 deaths per 100,000 live births.
Maternal Mortality in the United States and Around the Globe
Maternal mortality is most often caused by hemorrhaging, both in the United States and globally. However, causes affecting the rate of maternal mortality tend to vary based on location.
In the United States, hemorrhage as well as cardiovascular and coronary conditions cause the most pregnancy-related deaths, followed by cardiomyopathy, infection, embolism, mental-health conditions, preeclampsia and eclampsia.
Around the world, hemorrhage, hypertensive disorders and sepsis are the three leading causes of maternal mortality. Hemorrhage causes 27.1 percent of pregnancy-related deaths globally, while hypertensive disorders and sepsis cause 14 and 10.7 percent, respectively.
U.S. MMR Factors
Approximately 42.6 percent of pregnancy-related deaths in the United States were patient-related, 34.8 percent were provider-related and 21.7 percent were related to the system of care.
Several factors may have an effect on maternal mortality, with the average pregnancy-related death having 3.7 critical contributing factors. The U.S.’ three leading causes of maternal mortality are hemorrhaging, cardiovascular and coronary conditions, and cardiomyopathy.
Hemorrhaging is responsible for 12.7 percent of pregnancy-related deaths. Factors that can contribute to hemorrhaging include a delay in diagnosis, the patient lacking knowledge of warning signs, an absence of established policies and procedures, care personnel lacking education and insufficient care coordination.
Cardiovascular and coronary conditions are responsible for 12.7 percent of maternal mortalities. Factors that can contribute to cardiovascular and coronary conditions include misdiagnosis, the patient lacking knowledge of warning signs, chronic conditions affecting the patient and communication issues with the provider.
Cardiomyopathy is responsible for 11.4 percent of pregnancy-related deaths. Factors that can contribute to cardiomyopathy include misdiagnosis, chronic conditions affecting the patient and neglecting to seek a cardiology consultation.
Reducing the MMR
A variety of steps can be taken to reduce the maternal mortality rate, several of which involve educating expectant mothers and taking recommended precautions.
Allowing all women to access care is especially important as uninsured and underinsured mothers may be vulnerable to receiving health care that is less than ideal. Offering health care that is both accessible and affordable enables women to receive the care they need.
Educating women about pregnancy health and providing access to contraception is another effective way to reduce the MMR. Knowing about pregnancy health, risky symptoms and safe abortion services allows women to protect themselves from pregnancy-related dangers.
Taking precautions before performing a cesarean delivery may also lower the maternal mortality rate. States reporting an above average rate of cesarean births had a 21 percent higher risk of pregnancy-related death than states reporting a below average rate of cesarean births.
As 45 percent of U.S. pregnancies are unplanned, many women fail to address chronic health issues early in the pregnancy. An estimated 58.9 percent of maternal-related deaths in the United States stem from preventable causes. However, practicing good hygiene habits and allowing health care providers to check for infection can reduce maternal mortality rates.
Providing health care providers with comprehensive education on the treatment of symptoms and possible emergencies is another way to mitigate risks during pregnancy. For example, the risk of hemorrhage and severe bleeding may be reduced with an oxytocin injection immediately after childbirth. Preeclampsia is another potentially life-threatening condition that may be treated using magnesium sulfate and other anti-seizure drugs, which can lower the risk of developing this complication.
While most developed countries are making strides in preventing maternal-related deaths, the United States is falling behind. Addressing the causes of maternal mortality as well as contributing factors and underlying problems is a national concern. Health care professionals are the first line of defense for reversing this lethal trend.
Recommended Readings
A Guide to The Health Benefits of Breast-feeding
What Does The Future of The Nursing Industry Look Like?
Bradley University Online MSN-FNP Program
